Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Scientific Reports volume 13, Article number: 22637 (2023 ) Cite this article Excessive Sleepiness
Subjective–objective discrepancies in sleep onset latency (SOL), which is often observed among psychiatric patients, is attributed partly to the definition of sleep onset. Recently, instead of SOL, latency to persistent sleep (LPS), which is defined as the duration from turning out the light to the first consecutive minutes of non-wakefulness, has been utilized in pharmacological studies. This study aimed to determine the non-awake time in LPS that is most consistent with subjective sleep onset among patients with psychiatric disorders. We calculated the length of non-awake time in 30-s segments from lights-out to 0.5–60 min. The root mean square error was then calculated to determine the most appropriate length. The analysis of 149 patients with psychiatric disorders showed that the optimal non-awake time in LPS was 12 min. On the other hands, when comorbid with moderate or severe obstructive sleep apnea (OSA), the optimal length was 19.5 min. This study indicates that 12 min should be the best fit for the LPS non-awake time in patients with psychiatric disorders. When there is comorbidity with OSA, however, a longer duration should be considered. Measuring LPS minimizes discrepancies in SOL and provides important clinical information.
Insomnia is one of the core symptoms of patients with psychiatric disorders1. Prolonged sleep onset latency (SOL) frequently occurs in various psychiatric disorders, with the residual insomnia symptoms including difficulty falling asleep, and having a negative impact on the treatment of psychiatric disorders2,3. Initiation of sleep involves a complex neural structures and neurotransmitters4,5. It begins with activation of the ventral lateral preoptic nucleus in the hypothalamus, which inhibits the arousal systems of the brainstem and forebrain4. Neurotransmitters involved include gamma-aminobutyric acid and galanin, which promote sleep, and histamine, norepinephrine, and serotonin, which are associated with wakefulness5. These mechanisms play an important role in sleep initiation, but subjective and objective sleep often diverge. Subjective and objective sleep assessments have been widely used to evaluate sleep, however, discrepancies between subjective and objective sleep durations are common in psychiatric patients, with this condition known as sleep state misperception6,7,8. Even when patients objectively get a regular amount of sleep, their sleep state misperception can cause worry and anxiety about sleep, thereby leading to an objective sleep disturbance9. Although the underlying mechanism of the sleep state misperception remains elusive, previous research has discovered several variables, such as cognitive and psychological factors, the ability to estimate time, physiological factors9,10,11.
In addition to the above, the definition and measurement of sleep onset could be related to the misperception of SOL9. According to the American Academy of Sleep Medicine (AASM), the definition of conventional SOL is the time from lights out to the start of the first epoch of any of the sleep stages (N1, N2, N3, rapid eye movement: REM)12. In contrast, a new concept of latency to persistent sleep (LPS) has been defined as the duration from turning out the light to the first consecutive minutes of non-wakefulness13. LPS is increasingly being used as a concept to measure SOL in developmental research on sleep drugs, as LPS has the advantage of being able to measure sleep persistence13,14. Since sleep in insomniacs is typically inconsistent, the assessment of continuous state of sleep onset for a defined period, such as the LPS, is likely to be more accurate than using the standard epoch measurements.
Although this LPS non-awake time is often set at 10 min, ranging from 5 to 34 min has been reported, no consistent findings have yet been obtained15,16,17,18,19,20. Furthermore, since most of these studies focused on primary insomnia, it has yet to be definitively determined as to how long this continuous length best reflects the subjective sleep onset in patients with psychiatric disorders, as these patients may have different sleep structures21,22. Therefore, this study attempted to find the most appropriate non-awake time in LPS among psychiatric patients in real-world clinical practice.
We conducted a cross-sectional single-center study. This study analyzed the data from patients who had undergone polysomnography (PSG) at Nagoya University Hospital from 2016 to 2022. Inclusion criteria were: (1) 18 years of age or over, (2) availability of subjective sleep estimation data, (3) complete sleep epoch data with no deficiencies, and (4) the patient met any of the criteria for psychiatric disorders based on DSM-5. Exclusion criteria were: (1) comorbid neurodegenerative diseases, (2) intellectual disability, (3) dementia or cognitive decline, (4) having undergone PSG while using a continuous positive airway pressure or oral appliance, (5) hypersomnia, and (6) central sleep apnea. Out of the 269 total patients, 149 patients met these criteria and were included in our analysis (Fig. 1). All diagnoses were made by several skilled psychiatrists and all participants had stables symptoms. Patients completed a self-administered questionnaire prior to performing the PSG, and estimated their subjective SOL in the morning after the PSG overnight. All procedures were approved by the Ethics Review Committees at Nagoya University Hospital. Written informed consent in compliance with the guidelines of the Declaration of Helsinki was provided by all patients and obtained prior to participation.
Procedure for recruitment of subjects. PSG polysomnography, CPAP continuous positive airway pressure.
The Pittsburgh Sleep Quality Index, which is a 19-item instrument that assesses subjective sleep quality, SOL, and total sleep time (TST), was used to assess sleep quality23. The questionnaire consists of seven elements, with a total score ranging from 0 to 21. Previous studies have reported that patients with a score of 6 or above were poor sleepers. In addition, we defined difficulty falling asleep based on the PSQI subscale as follows: SOL for question 2 was more than 30 min, while the answer for question 5a regarding the number of times a patient could not get to sleep being reported as “three or more times per week.
This investigation utilized a standard PSG (Embla N7000, Natus Neurology Incorporated, WI, USA or PSG-1100, Nihon Kohden Co., Tokyo, Japan). The AASM scoring manual, version 2.1, was used to assess the results12. Details for these techniques have been previously published24. Trained sleep technologists evaluated the TST, SOL, and apnea–hypopnea index (AHI). PSG recordings were consistently conducted over an 8-h period. Specifically, the recordings were carried out either from 9 p.m. to 5 a.m. or from 10 p.m. to 6 a.m.
After completing the PSG in the morning, participants were asked to estimate their subjective SOL using the following question: “How long did it take you to fall asleep?”. Participants then provided their SOL in hours and minutes.
The duration of the first sleep epoch after turning out the lights and the specific sustained non-awake time were calculated in this study based on the data from each participant that were collected in 30 s increases, which ranged from 0.5 to 60 min of no interrupted sleep. If an awakening epoch was observed during the monitored sleep period, this sleep period was not considered to be continuous sleep18.
All data except for age and score of PSQI are presented as the median and interquartile range (IQR). Root mean square error (RMSE) was calculated between the subjective SOL and each LPS with a non-awake time of 0.5–60 min. Then, we plotted the RMSE on a graph in order to detect the most suitable value for the sleep duration. A lower RMSE indicated that there was no difference between the two sleep measurements. All statistical analyses in this study were performed using R 4.1.1.
Table 1 presents the patient’s clinical characteristics. In total, 149 patients were evaluated (89 males, 60 females), with a mean age of 47.2 years (SD 16.8 years). The prevalence of the psychiatric disorders was as follows: major depressive disorders (n = 45, 30%), bipolar disorders (n = 34, 23%), neurodevelopmental disorders (n = 29, 19%), schizophrenia (n = 14, 9.4%), somatic disorders (n = 12, 8.1%), other disorders (n = 10, 6.7%), and anxiety disorders (n = 5, 3.4%). For sleep disorders, these included: obstructive sleep apnea (OSA) (n = 99, 64%), periodic limb movement disorder (PLMD) (n = 4, 2.7%), REM sleep behavior disorder (RBD) (n = 3, 2.0%), and restless legs syndrome (RLS) (n = 1, 0.7%). The prevalence of medication use among participants was as follows: benzodiazepines were the most commonly used (n = 64, 43.0%), followed by Antipsychotics (n = 59, 39.6%), Antidepressants (n = 55, 36.9%), Hypnotic (n = 45, 30.2%), Mood stabilizers (n = 31, 20.8%), and Anti-Parkinson drugs (n = 1, 0.7%).
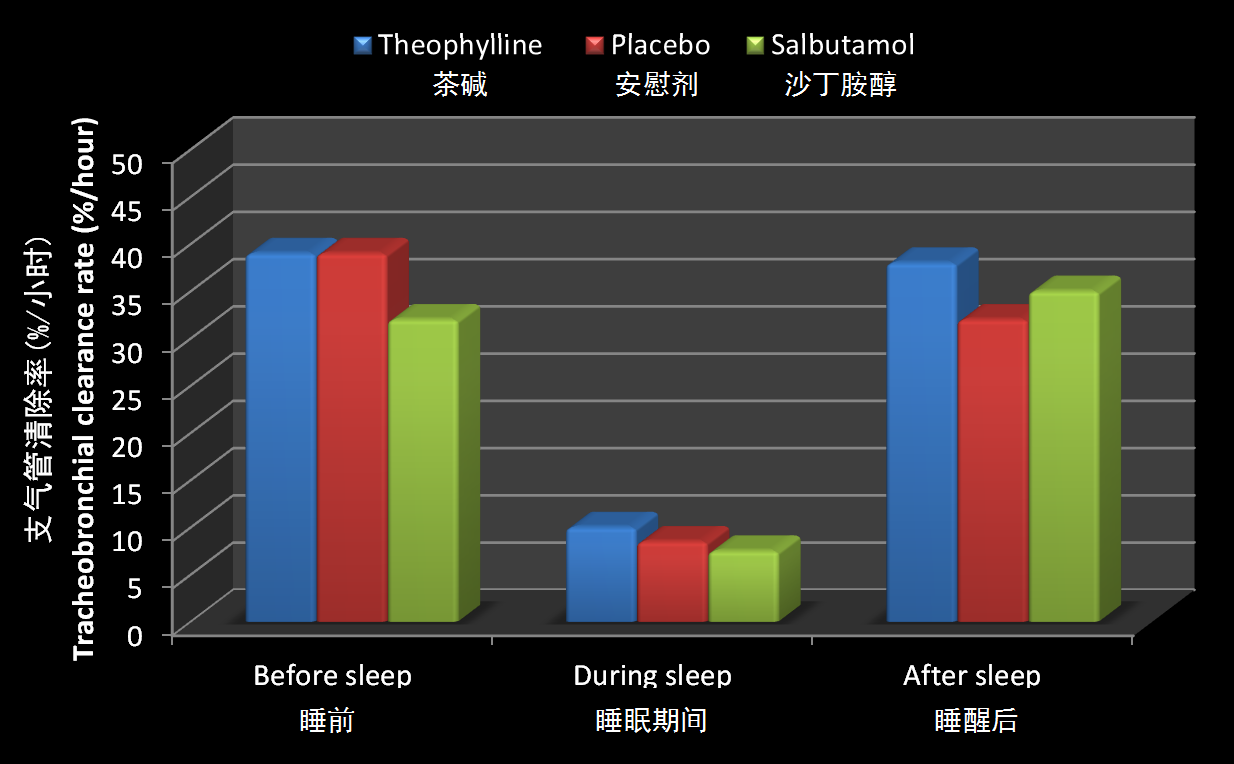
LPS was calculated based on each non-awake time, with the RMSEs calculated from the subjective SOL and each LPS with a non-awake time of 0.5–60 min in order to identify the optimal sleep duration for the latency (Fig. 2). An RMSE of 12 min of sleep duration was the lowest value found for all of the psychiatric patients’ data (Fig. 2A, n = 149). Based on these data, we then calculated the RMSEs for those patients who reported having subjective insomnia symptoms and those who did not, respectively, as indicated by the PSQI. Figure 2B (n = 120) indicated that those with subjective insomnia had the lowest RMSE at 13 min, while Fig. 2C (n = 29) shows that the lowest RMSE in patients without subjective insomnia was 8.5 min. After adding the symptoms of difficulty falling asleep, the lowest RMSE for those patients suffering from this issue was 13–13.5 min as compared to 13 min for those who did not have this issue (Fig. 2D, n = 54, Fig. 2E, n = 66). We also calculated the RMSE for subjective insomnia symptoms combined with moderate or severe OSA The RMSE was smallest at 19.5 min when insomnia symptoms were comorbid with moderate or severe OSA, and 10.5 min when no OSA was comorbid (Fig. 2F, n = 37, Fig. 2G, n = 83).
The RMSE outcomes between subjective SOL and LPS. The x-axis represents the length of non-awake time (min). The y-axis represents the RMSE. (A) For all participants (n = 149), the optimal length of non-awake time was 12 min. (B) For participants with subjective insomnia (n = 120), the optimal length of non-awake time was 13 min. (C) For participants without subjective insomnia (n = 29), the optimal length of non-awake time was 8.5 min. (D) For participants with subjective insomnia and difficulty in falling asleep (n = 54), the optimal length of non-awake time was 13–13.5 min. (E) For participants with subjective insomnia but no difficulty in falling asleep (n = 66), the optimal length of non-awake time was 13 min. (F) For participants with subjective insomnia and moderate or severe OSA (n = 37), the optimal length of non-awake time was 19.5 min. (G) For participants with subjective insomnia and no OSA (n = 83), the optimal length of non-awake time was 10 min. RMSE root mean square error, SOL sleep onset latency, OSA obstructive sleep apnea, TST total sleep time, SOL sleep onset latency, WASO wake after sleep onset, AHI apnea hypopnea index, PSQI Pittsburgh Sleep Quality Index, OSA obstructive sleep apnea, PLMD periodic limb movement disorders, RBD rapid eye movement sleep behavior disorders, RLS restless legs syndrome, PLMI periodic leg movement during sleep index, PSG polysomnography, CPAP continuous positive airway pressure, RMSE root mean square error, REM rapid eye movement, LPS latency to persistent sleep, IQR interquartile range.
The aim of this study was to determine the most appropriate non-awake time that is concordant with the subjective SOL in patients with psychiatric disorders. Our results revealed that among all of the psychiatric patients, the duration from the lights out to 12 uninterrupted minutes of LPS non-awake time was an optimal length. In addition, among psychiatric patients with moderate or severe OSA, 19.5 LPS non-awake time was the most optimal. These findings demonstrate the importance of measuring LPS as a way to minimize overestimation of SOL.
The 12-min length was roughly approximate to the current duration of LPS non-awake time that is used in clinical settings. Carskadon19 proposed the first consecutive 10-min sleep epoch latency that occurs from lights out to falling asleep. A previous study reported that the concordance between the subjective and objective SOL was optimal when the first epoch of N2 lasted for at least 15 min20. However, other suggested 34 and 22 min as the optimal non-wakefulness for insomniac and normal subjects, respectively18. One possible reason for this discrepancy is that the original subjective and objective SOL in our participants were shorter than that observed for the other studies. The median subjective and objective SOL for insomniacs was 123 and 25 min, respectively, whereas our median subjective and objective SOL for psychiatric patients was 30 and 10.5 min, respectively. Even among patients with psychiatric disorders who reported subjective insomnia, the median subjective SOL was 42.5 min while the median objective SOL was 11.75 min. Thus, differences found in the SOL of our sample may have led to the differences observed from the previous studies.
Furthermore, we demonstrated that the existence of OSA and its severity may prolong the LPS non-awake time. Previous studies have reported that the OAS was associated with SOL overestimation. In other words, patients with OSA have shorter objective SOL and longer subjective SOL25. A possible mechanism for this could be associated with the relationship found between sleepiness and the OSA. Results of studies that have investigated SOL and sleepiness in OSA patients suggested that higher daytime sleepiness was associated with shorter objective SOL26,27. These results suggested that the high levels of daytime sleepiness observed in patients with OSA increases sleep pressure and may have shorten the time it takes to fall asleep. Moreover, patients with OSA have been reported to have more awakenings during sleep, with more unstable sleep stages observed as compared to patients without OSA28,29. In other words, it's possible that people with OSA fall asleep faster due to their daily sleepiness, but they experience awaking after they fall asleep. Based on these previous findings, the current sleep index, which is the duration between the turning out of the lights and the onset of a particular stage of sleep as measured in a 30-s epoch, may ignore the awakenings that occur after judgement of falling sleep. Furthermore, one experimental study reported finding that by suppressing breathing during sleep onset, participants were not aware of the subjective falling asleep, even if the stageN2 condition lasted for 25 min30. Therefore, this widely used optimal length for sleep onset decisions appears to be longer than the ten consecutive minutes currently being used.
There are several strengths of our study. First, to the best of our knowledge, this is the first study to have investigated the LPS non-awake time among patients with psychiatric disorders. Second, the length that we define in our study takes into consideration the comorbidity with OSA, which is found in a high prevalence of psychiatric patients31.
However, there were also several limitations of the present study. First, the subgroup analysis for each of the psychiatric disorders was impossible to carry out due to the small sample size of this study. Furthermore, we were unable to establish a control group. Second, the results of our study were not completely adjusted for the effects of psychiatric drugs, as many of the participants took multiple drugs, not just one drug. Since previous studies have reported on some of the effects of psychiatric drugs on sleep32,33,34, it will be necessary to further investigate how the type of drug and dosage can affect the findings of this type of research. Third, the measurements of the sleep of all participants were collected under controlled conditions. Thus, these results should be viewed with some caution, as measurements of sleep when obtained in home settings could very well be different from those obtained in a laboratory setting. Finally, we did not collect the data on their habit of nap. Taking nap can deprive sleep pressure and it would influence on sleep onset latency, although short naps do not have much of an effect35,36. Future research will need to examine the relationship between these findings and additional indices, including psychological and symptom rating scales while considering other confounders such as usual sleep habits and gender difference.
In conclusion, the appropriate LPS non-awake time among psychiatric patients was 12 min, which was not largely different from the existing length of 10-min LPS currently being utilized in other settings. However, the length of consecutive sleep for the purpose of calculating a sleep score can be longer for subjects that are comorbid with moderate or severe OSA. These findings can facilitate more accurate sleep assessment and appropriate treatment decisions in actual clinical practice, and may be one of the factors that minimize misperception of SOL.
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Krystal, A. D. Psychiatric disorders and sleep. Neurol. Clin. 30, 1389–1413. https://doi.org/10.1016/j.ncl.2012.08.018 (2012).
Article PubMed PubMed Central Google Scholar
Sakurai, H., Suzuki, T., Yoshimura, K., Mimura, M. & Uchida, H. Predicting relapse with individual residual symptoms in major depressive disorder: A reanalysis of the STAR*D data. Psychopharmacology (Berlin) 234, 2453–2461. https://doi.org/10.1007/s00213-017-4634-5 (2017).
Plante, D. T. & Winkelman, J. W. Sleep disturbance in bipolar disorder: Therapeutic implications. Am. J. Psychiatry 165, 830–843. https://doi.org/10.1176/appi.ajp.2008.08010077 (2008).
España, R. A. & Scammell, T. E. Sleep neurobiology from a clinical perspective. Sleep 34, 845–858. https://doi.org/10.5665/sleep.1112 (2011).
Article PubMed PubMed Central Google Scholar
Omond, S. E. T., Hale, M. W. & Lesku, J. A. Neurotransmitters of sleep and wakefulness in flatworms. Sleep. https://doi.org/10.1093/sleep/zsac053 (2022).
Article PubMed PubMed Central Google Scholar
Rezaie, L., Fobian, A. D., McCall, W. V. & Khazaie, H. Paradoxical insomnia and subjective-objective sleep discrepancy: A review. Sleep Med. Rev. 40, 196–202. https://doi.org/10.1016/j.smrv.2018.01.002 (2018).
Castelnovo, A. et al. The paradox of paradoxical insomnia: A theoretical review towards a unifying evidence-based definition. Sleep Med. Rev. 44, 70–82. https://doi.org/10.1016/j.smrv.2018.12.007 (2019).
Kawai, K. et al. A study of factors causing sleep state misperception in patients with depression. Nat. Sci. Sleep 14, 1273–1283. https://doi.org/10.2147/NSS.S366774 (2022).
Article PubMed PubMed Central Google Scholar
Harvey, A. G. & Tang, N. K. (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychol. Bull. 138, 77–101. https://doi.org/10.1037/a0025730 (2012).
Tang, N. K. & Harvey, A. G. Effects of cognitive arousal and physiological arousal on sleep perception. Sleep 27, 69–78. https://doi.org/10.1093/sleep/27.1.69 (2004).
Hermans, L. W. A., Nano, M. M., Leufkens, T. R., van Gilst, M. M. & Overeem, S. Sleep onset (mis)perception in relation to sleep fragmentation, time estimation and pre-sleep arousal. Sleep Med. X 2, 100014. https://doi.org/10.1016/j.sleepx.2020.100014 (2020).
Article PubMed PubMed Central Google Scholar
Berry, R.B., Albertario, C.L., Harding, S. & Gamaldo, C. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications, version 2. Darien, IL. Am. Acad. Sleep Med. (2018).
Rosenberg, R. et al. Comparison of lemborexant with placebo and zolpidem tartrate extended release for the treatment of older adults with insomnia disorder: A phase 3 randomized clinical trial. JAMA Netw. Open 2, e1918254. https://doi.org/10.1001/jamanetworkopen.2019.18254 (2019).
Article PubMed PubMed Central Google Scholar
Pinto, L. R., SeabraMde, L. & Tufik, S. Different criteria of sleep latency and the effect of melatonin on sleep consolidation. Sleep 27, 1089–1092. https://doi.org/10.1093/sleep/27.6.1089 (2004).
Rechstchaffen AA, K. A. A Manual of Standardized Terminology Techniques and Scoring System for Sleep Stages of Human Subjects. Los Angeles. (Brain Information Service/Brain Research Institute, 1968).
Webb, W. B. Recording methods and visual scoring criteria of sleep records: Comments and recommendations. Percept. Mot. Skills 62, 664–666. https://doi.org/10.2466/pms.1986.62.2.664 (1986).
Article CAS PubMed Google Scholar
Hermans, L. W. A. et al. Sleep EEG characteristics associated with sleep onset misperception. Sleep Med. 57, 70–79. https://doi.org/10.1016/j.sleep.2019.01.031 (2019).
Hermans, L. W. A. et al. Modeling sleep onset misperception in insomnia. Sleep. https://doi.org/10.1093/sleep/zsaa014 (2020).
Carskadon, M.A., R. A. Princ. Pract. Sleep Med. 1197–1215 (2000).
Hauri, P. & Olmstead, E. What is the moment of sleep onset for insomniacs?. Sleep 6, 10–15. https://doi.org/10.1093/sleep/6.1.10 (1983).
Article CAS PubMed Google Scholar
Baglioni, C. et al. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 142, 969–990. https://doi.org/10.1037/bul0000053 (2016).
Article PubMed PubMed Central Google Scholar
Staner, L. et al. Sleep microstructure around sleep onset differentiates major depressive insomnia from primary insomnia. J. Sleep Res. 12, 319–330. https://doi.org/10.1046/j.0962-1105.2003.00370.x (2003).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Article CAS PubMed Google Scholar
Fujishiro, H. et al. Early diagnosis of Lewy body disease in patients with late-onset psychiatric disorders using clinical history of rapid eye movement sleep behavior disorder and [(123) I]-metaiodobenzylguanidine cardiac scintigraphy. Psychiatry Clin. Neurosci. 72, 423–434. https://doi.org/10.1111/pcn.12651 (2018).
Article CAS PubMed Google Scholar
Saline, A., Goparaju, B. & Bianchi, M. T. Sleep fragmentation does not explain misperception of latency or total sleep time. J. Clin. Sleep Med. 12, 1245–1255. https://doi.org/10.5664/jcsm.6124 (2016).
Article PubMed PubMed Central Google Scholar
Sun, Y. et al. Polysomnographic characteristics of daytime sleepiness in obstructive sleep apnea syndrome. Sleep Breath 16, 375–381. https://doi.org/10.1007/s11325-011-0515-z (2012).
Mediano, O. et al. Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur. Respir. J. 30, 110–113. https://doi.org/10.1183/09031936.00009506 (2007).
Article CAS PubMed Google Scholar
Bianchi, M. T., Cash, S. S., Mietus, J., Peng, C. K. & Thomas, R. Obstructive sleep apnea alters sleep stage transition dynamics. PLoS One 5, 1–12. https://doi.org/10.1371/journal.pone.0011356 (2010).
Bianchi, M. T., Williams, K. L., McKinney, S. & Ellenbogen, J. M. The subjective-objective mismatch in sleep perception among those with insomnia and sleep apnea. J. Sleep Res. 22, 557–568. https://doi.org/10.1111/jsr.12046 (2013).
Smith, S. & Trinder, J. The effect of arousals during sleep onset on estimates of sleep onset latency. J. Sleep Res. 9, 129–135. https://doi.org/10.1046/j.1365-2869.2000.00194.x (2000).
Article CAS PubMed Google Scholar
Okada, I. et al. Prevalence of obstructive sleep apnea as assessed by polysomnography in psychiatric patients with sleep-related problems. Sleep Breath. https://doi.org/10.1007/s11325-022-02566-6 (2022).
Monti, J. M., Torterolo, P. & Pandi Perumal, S. R. The effects of second generation antipsychotic drugs on sleep variables in healthy subjects and patients with schizophrenia. Sleep Med. Rev. 33, 51–57. https://doi.org/10.1016/j.smrv.2016.05.002 (2017).
Hutka, P. et al. Association of sleep architecture and physiology with depressive disorder and antidepressants treatment. Int. J. Mol. Sci. https://doi.org/10.3390/ijms22031333 (2021).
Article PubMed PubMed Central Google Scholar
Atkin, T., Comai, S. & Gobbi, G. Drugs for insomnia beyond benzodiazepines: Pharmacology, clinical applications, and discovery. Pharmacol. Rev. 70, 197–245. https://doi.org/10.1124/pr.117.014381 (2018).
Article CAS PubMed Google Scholar
Owens, J. F. et al. Napping, nighttime sleep, and cardiovascular risk factors in mid-life adults. J. Clin. Sleep Med. 6, 330–335 (2010).
Article PubMed PubMed Central Google Scholar
Brooks, A. & Lack, L. A brief afternoon nap following nocturnal sleep restriction: Which nap duration is most recuperative?. Sleep 29, 831–840. https://doi.org/10.1093/sleep/29.6.831 (2006).
We would like to thank all of the patients for their participation in this research. This research was supported by AMED under Grants JP20dk0307099 and JP22dk0307113 and JSPS KAKENHI Grant nos. JP17K10272 and JP21K07518.
Department of Psychiatry, Nagoya University Graduate School of Medicine, 65 Tsurumai-Cho, Showa, Nagoya, Aichi, 466-8550, Japan
Keita Kawai, Kunihiro Iwamoto, Seiko Miyata, Ippei Okada, Motoo Ando, Hiroshige Fujishiro & Norio Ozaki
Department of Advanced Medicine, Nagoya University Hospital, Nagoya, Aichi, Japan
Department of Biomedical Sciences, Chubu University Graduate School of Life and Health Sciences, Kasugai, Aichi, Japan
Pathophysiology of Mental Disorders, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
K.K.: study design, statistical analysis, data interpretation, data acquisition, and writing and editing of the manuscript. K.I., S.M.: study design, data interpretation, data acquisition, and writing and editing of the manuscript. I.O., M.O.: data acquisition, and writing and editing of the manuscript. H.F.: writing and editing of the manuscript. M.A.: study design, statistical analysis, data interpretation, and writing and editing of the manuscript. A.N.: writing and editing of the manuscript. N.O.: study design, and writing and editing of the manuscript.
KI has received speakers’ honoraria from Eisai, Kyowa, Meiji Seika Pharma, MSD, Otsuka, Sumitomo Pharma, Taisho, Takeda, Towa, and Viatris. MA has received subsidies from Kyowa Kirin. NO received research support or speakers’ honoraria from, or have served as a consultant to, Sumitomo Dainippon, Eisai, Otsuka, KAITEKI, Mitsubishi Tanabe, Shionogi, Eli Lilly, Mochida, Daiichi Sankyo, Nihon Medi-Physics, Takeda, Meiji Seika Pharma, EA Pharma, Pfizer, MSD, Lundbeck Japan, Taisho Pharma, Janssen, UCB and Shionogi, Tsumura, Novartis, and Astellas.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Kawai, K., Iwamoto, K., Miyata, S. et al. LPS and its relationship with subjective–objective discrepancies of sleep onset latency in patients with psychiatric disorders. Sci Rep 13, 22637 (2023). https://doi.org/10.1038/s41598-023-49261-4
DOI: https://doi.org/10.1038/s41598-023-49261-4
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Scientific Reports (Sci Rep) ISSN 2045-2322 (online)
Insomnia During Pregnancy Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.