Don't miss the latest content from this profile: log in to be able to add new content from profiles and districts to your personal favourites.
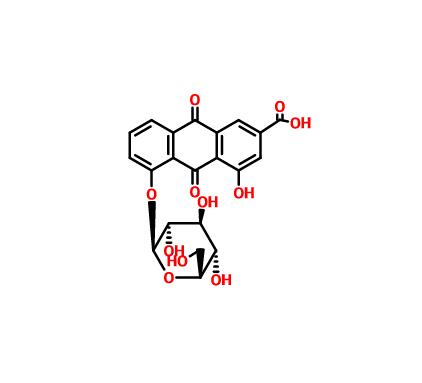
ANFELDEN (red).The individual state championships in squash were recently held in the Obtus sports park in Ansfelden.In the women's race, Ansfelden athlete Karolin Wabro was able to beat last year's national champion Anita Kafko 3:1 in the final and bring the national championship title to Ansfelden. Vitexin
In the men's category, the only 16-year-old Paul Mairinger from the SquashClub Haid/Ansfelden once again put in a sovereign test of talent and, after clear victories in the preliminary round, made it through to the final.After hard-fought sentences, Paul had to admit defeat against multiple national champion Daniel Haider, but was able to celebrate his first podium finish at national championships.
The mayor of Ansfelden, Manfred Baumberger, was also enthusiastic about the action-packed games and the emotionally charged atmosphere when he visited the Obermayr sports park.
Sign in to like this content.
Would you like to contribute to the discussion?Sign in to post comments.
Irisolidone Register now for free to contribute your own content.